Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering...Read more
Breast reduction surgery is a popular cosmetic procedure that helps women alleviate the physical discomfort associated with having large breasts. However, the high cost of this surgery often discourages individuals from seeking it out. For those who are covered by Medicaid, the question of whether the program can pay for breast reduction surgery arises. This is a complex issue that requires an understanding of Medicaid policies and regulations.
Medicaid is a government-funded program that provides health coverage to low-income individuals and families. While it covers a wide range of medical procedures, cosmetic surgeries such as breast reduction are generally not covered unless they are deemed medically necessary. In this article, we will explore the requirements for Medicaid coverage of breast reduction surgery, the criteria used to determine medical necessity, and the steps individuals can take to increase their chances of receiving coverage.
Contents
- Can Medicaid Pay for Breast Reduction?
- Frequently Asked Questions
- Can Medicaid cover breast reduction surgery?
- What criteria must be met for Medicaid to cover breast reduction surgery?
- What costs are covered by Medicaid for breast reduction surgery?
- How can I apply for Medicaid coverage for breast reduction surgery?
- What should I expect during the Medicaid approval process for breast reduction surgery?
- Will insurance cover breast reduction surgery?
- Can I Keep Medicaid If My Job Offers Insurance?
- Does Smile Direct Club Take Medicaid Insurance?
- Does Life Insurance Payout Affect Medicaid?
Can Medicaid Pay for Breast Reduction?
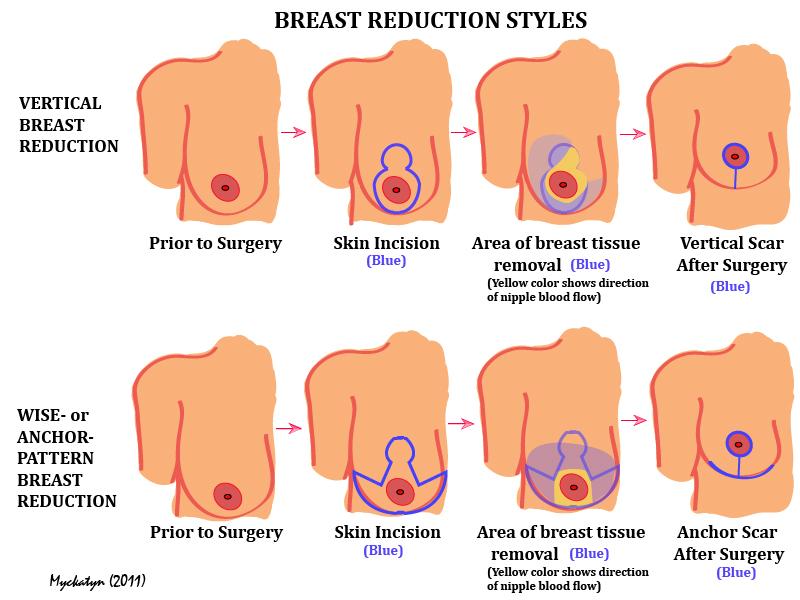
Breast reduction surgery, also known as reduction mammoplasty, is a surgical procedure performed to remove excess breast tissue, skin, and fat to achieve a more proportional breast size. Women with overly large breasts often experience pain, discomfort, and difficulty performing everyday activities. While breast reduction surgery is a viable solution to alleviate these symptoms, the cost of the procedure can be a significant hurdle for many women. Fortunately, for those who qualify, Medicaid may cover the cost of breast reduction surgery.
What is Medicaid?
Medicaid is a government-funded healthcare program that provides medical assistance to eligible individuals with low incomes and limited resources. The program is administered by the states and covers a range of medical services, including doctor visits, hospital stays, prescription drugs, and surgical procedures. Medicaid eligibility requirements vary by state, but generally, individuals with incomes up to 138% of the federal poverty level are eligible for coverage.
Does Medicaid Cover Breast Reduction Surgery?
Medicaid does cover breast reduction surgery, but only under certain circumstances. Generally, breast reduction surgery is considered a cosmetic procedure and therefore not covered by Medicaid. However, if the surgery is deemed medically necessary to treat a condition such as chronic back pain or skin irritation, Medicaid may cover the cost of the procedure.
To qualify for Medicaid coverage of breast reduction surgery, you must meet certain criteria. Your doctor will need to document that you have a medical condition related to your breast size and that other treatments, such as physical therapy or pain medication, have been ineffective in relieving your symptoms. Additionally, your doctor will need to provide evidence that breast reduction surgery will significantly improve your condition.
Benefits of Breast Reduction Surgery
Breast reduction surgery offers many benefits beyond just cosmetic improvement. Women who undergo the procedure often experience relief from chronic back, neck, and shoulder pain, as well as skin irritation and rashes caused by large breasts. Breast reduction surgery can also improve posture and increase mobility, making it easier to perform everyday activities like exercise and housework.
Breast Reduction Surgery Vs. Breast Lift
Breast reduction surgery and breast lift surgery are two different procedures that can be confused with one another. While both procedures involve altering the appearance of the breasts, they serve different purposes. Breast reduction surgery is performed to remove excess breast tissue, skin, and fat to reduce the size of the breasts. Breast lift surgery, on the other hand, is performed to lift and reshape sagging breasts.
If you are considering breast surgery, it is important to consult with a qualified plastic surgeon to determine which procedure is right for you. Your surgeon will evaluate your individual needs and goals and recommend the best course of action.
Conclusion
Breast reduction surgery can be life-changing for women who suffer from the physical and emotional discomforts associated with overly large breasts. While the cost of the procedure can be a barrier to access for many women, Medicaid may cover the cost of the surgery if it is deemed medically necessary. If you are considering breast reduction surgery, it is important to discuss your options with a qualified healthcare provider and explore all available resources to make the procedure more affordable.
Frequently Asked Questions
Here are some common questions and answers about whether Medicaid can pay for breast reduction surgery:
Can Medicaid cover breast reduction surgery?
Yes, Medicaid can cover breast reduction surgery if it is deemed medically necessary by a healthcare professional. This means that the surgery must be recommended to alleviate physical pain or discomfort caused by excessively large breasts. Medicaid will not cover the procedure if it is solely for cosmetic reasons.
It is important to note that each state has its own eligibility requirements and coverage limitations. It is recommended to contact your state’s Medicaid office to determine if you qualify for coverage and what specific services are covered.
What criteria must be met for Medicaid to cover breast reduction surgery?
Medicaid will typically cover breast reduction surgery if it is deemed medically necessary. This means that the surgery must be recommended to alleviate physical pain or discomfort caused by excessively large breasts. In addition, the patient must have tried alternative treatments, such as physical therapy or pain medication, with no relief.
It is important to note that each state has its own eligibility requirements and coverage limitations. It is recommended to contact your state’s Medicaid office to determine if you qualify for coverage and what specific services are covered.
What costs are covered by Medicaid for breast reduction surgery?
Medicaid will typically cover the costs associated with breast reduction surgery, including surgeon fees, anesthesia, and hospitalization. However, there may be limitations on the amount of coverage and certain services may not be covered. For example, some states may not cover the cost of implants or the cost of surgery for purely cosmetic reasons.
It is important to contact your state’s Medicaid office to determine what specific services are covered and any out-of-pocket costs that may be required.
How can I apply for Medicaid coverage for breast reduction surgery?
To apply for Medicaid coverage for breast reduction surgery, you will need to contact your state’s Medicaid office. They will provide you with information on how to apply and what documentation is required. You will typically need to provide medical documentation that supports the need for the surgery.
It is important to note that each state has its own eligibility requirements and coverage limitations. It is recommended to contact your state’s Medicaid office to determine if you qualify for coverage and what specific services are covered.
What should I expect during the Medicaid approval process for breast reduction surgery?
The Medicaid approval process for breast reduction surgery can vary depending on the state and individual case. Typically, you will need to provide medical documentation that supports the need for the surgery. This can include a referral from a healthcare professional, medical records, and imaging tests.
Once your application is submitted, it will be reviewed by the Medicaid office. They may request additional information or documentation. If approved, you will receive notification of coverage and any out-of-pocket costs that may be required. If denied, you may have the option to appeal the decision.
Will insurance cover breast reduction surgery?
In conclusion, the question of whether Medicaid can pay for breast reduction is a complex one. While Medicaid does cover some procedures related to breast health, such as mastectomies and breast reconstruction following cancer treatment, breast reduction is generally considered a cosmetic procedure and is not covered unless it is deemed medically necessary.
However, it is important to note that each state may have its own guidelines and regulations regarding Medicaid coverage for breast reduction. Additionally, there may be certain circumstances, such as chronic pain or other medical issues related to large breasts, that could make breast reduction a covered procedure under Medicaid. As with any medical treatment, it is important to consult with a qualified healthcare provider and Medicaid representative to determine eligibility and coverage options.
Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering individuals to make well-informed decisions. Guided by his passion, he has assembled a team of seasoned insurance professionals committed to simplifying the intricate world of insurance for you.
- Latest Posts by Rakibul Hasan
-
Can I Keep Medicaid If My Job Offers Insurance?
- -
Does Smile Direct Club Take Medicaid Insurance?
- -
Does Life Insurance Payout Affect Medicaid?
- All Posts
