Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering...Read more
Medicaid is a government-funded health insurance program that helps millions of low-income individuals and families access the medical care they need. One of the most common questions people ask about Medicaid is whether or not it covers frenectomy, a surgical procedure that is used to treat conditions such as tongue-tie and lip-tie. If you or a loved one is considering a frenectomy, it is important to understand what Medicaid covers and how to navigate the system.
While Medicaid does cover a wide range of medical services, the coverage for frenectomy can vary depending on the state you live in and the specific circumstances of your case. In some states, Medicaid will cover the cost of frenectomy for children under a certain age, while in others it may only be covered for certain medical conditions. This can make it difficult for families to know what to expect when it comes to paying for this important medical procedure. In this article, we will explore the ins and outs of Medicaid coverage for frenectomy, so that you can make informed decisions about your health and the health of your loved ones.
Yes, Medicaid covers Frenectomy in certain cases. Frenectomy is a dental procedure that involves the removal or modification of the frenum, a small fold of tissue that connects the lips, tongue, or cheeks to the gums. Medicaid provides coverage for Frenectomy when it is deemed medically necessary to treat a patient’s oral health condition. However, coverage may vary by state and individual circumstances. It’s best to check with your Medicaid provider or dentist to confirm coverage.
Does Medicaid Cover Frenectomy?
What is a Frenectomy?
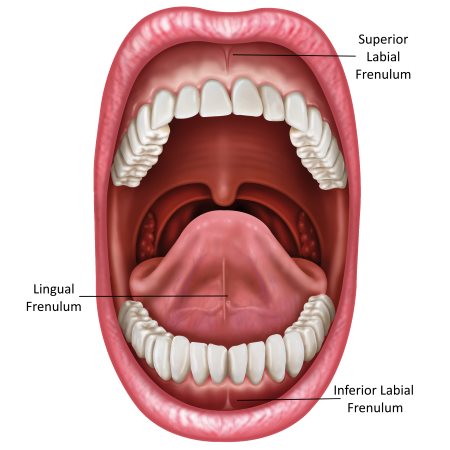
A frenectomy is a surgical procedure that removes the frenulum, which is a small fold of tissue that connects the lips, tongue, or cheeks to the gums or floor of the mouth. There are two types of frenectomy: lingual frenectomy, which is the removal of the frenulum under the tongue, and labial frenectomy, which is the removal of the frenulum that attaches the upper lip to the gums.
Why is a Frenectomy Needed?
A frenectomy is usually performed to treat a condition called ankyloglossia, commonly known as tongue-tie. Tongue-tie occurs when the frenulum under the tongue is too short or too tight, which restricts the movement of the tongue. This can lead to difficulty with breastfeeding, speaking, and swallowing. A frenectomy can also be performed to treat a condition called a lip-tie, which occurs when the frenulum that connects the upper lip to the gums is too short or too tight, which can cause problems with breastfeeding and speech.
Does Medicaid Cover Frenectomy?
The short answer is yes, Medicaid does cover frenectomy for eligible individuals. Medicaid is a federal and state-funded program that provides health insurance for low-income individuals and families. Each state has its own Medicaid program, and the coverage and eligibility requirements vary by state.
In general, Medicaid covers medically necessary services, including surgical procedures like frenectomy, as long as they are deemed medically necessary by a healthcare professional. However, coverage may be limited to certain types of frenectomy or may require prior authorization from the Medicaid program.
Benefits of Frenectomy
A frenectomy can have several benefits, including:
- Improved breastfeeding for infants
- Improved speech and pronunciation
- Improved oral hygiene
- Reduced risk of gum recession and periodontal disease
Frenectomy vs. Alternative Treatments
There are several alternative treatments for tongue-tie and lip-tie, including speech therapy, dental appliances, and myofunctional therapy. However, these treatments may not be as effective as frenectomy and may not be covered by Medicaid.
Speech therapy can help improve speech and pronunciation, but it may not address the underlying issue of tongue-tie or lip-tie. Dental appliances, such as orthodontic devices or tongue retainers, may help with certain symptoms but may not be a permanent solution. Myofunctional therapy focuses on improving tongue and facial muscle function through exercises but may not be effective for severe cases of tongue-tie or lip-tie.
How to Determine Eligibility for Medicaid Coverage
To determine eligibility for Medicaid coverage of frenectomy, individuals should contact their state Medicaid program or healthcare provider. Eligibility requirements vary by state but generally include income and household size. Medicaid may also cover frenectomy for individuals with certain medical conditions or disabilities.
If approved for Medicaid coverage, individuals should work with their healthcare provider to determine the best course of treatment for their specific case of tongue-tie or lip-tie.
Conclusion
In summary, Medicaid does cover frenectomy for eligible individuals as a medically necessary procedure. Frenectomy can have several benefits for individuals with tongue-tie or lip-tie, including improved breastfeeding, speech, and oral hygiene. While there are alternative treatments available, frenectomy may be the most effective and permanent solution. Individuals should contact their state Medicaid program or healthcare provider to determine eligibility and the best course of treatment for their specific case.
Contents
- Frequently Asked Questions
- What is a Frenectomy?
- Does Medicaid Cover Frenectomy?
- How much does a Frenectomy cost?
- What are the risks of a Frenectomy?
- How long does it take to recover from a Frenectomy?
- Is Medicaid Coverage Better or Worse than Private Insurance?
- Can I Keep Medicaid If My Job Offers Insurance?
- Does Smile Direct Club Take Medicaid Insurance?
- Does Life Insurance Payout Affect Medicaid?
Frequently Asked Questions
What is a Frenectomy?
A Frenectomy is a surgical procedure that involves the removal of a small piece of tissue called a frenum. This tissue can be found in various parts of the body, including the mouth, and can cause problems such as speech difficulties or dental issues if it is too tight or short.
The procedure is typically performed by an oral surgeon or dentist, and can be done with a scalpel, laser or other surgical tools. It is a relatively simple and straightforward procedure that can be done in-office, under local anesthesia.
Does Medicaid Cover Frenectomy?
Yes, Medicaid does cover Frenectomy. However, coverage may vary depending on the state and the specific circumstances of the patient. In general, Medicaid covers medically necessary procedures, and a Frenectomy can be considered medically necessary if it is causing problems with speech, eating or other oral functions.
Patients who are eligible for Medicaid should check with their provider to see if a Frenectomy is covered under their plan. They may also need to provide documentation from their dentist or oral surgeon to show that the procedure is necessary.
How much does a Frenectomy cost?
The cost of a Frenectomy can vary depending on the location, the type of procedure, and the provider performing the procedure. However, in general, the cost of a Frenectomy can range from $500 to $1,000 without insurance.
If a patient has Medicaid, the cost of the procedure may be covered. Patients should check with their provider to see if a Frenectomy is covered under their plan and if there are any out-of-pocket costs associated with the procedure.
What are the risks of a Frenectomy?
Like any surgical procedure, there are risks associated with a Frenectomy. These risks can include bleeding, infection, and damage to surrounding tissues or nerves. However, these risks are relatively low, and most patients experience a quick and easy recovery.
Patients who are considering a Frenectomy should talk to their dentist or oral surgeon about the risks and benefits of the procedure, and any potential complications that may arise.
How long does it take to recover from a Frenectomy?
The recovery time for a Frenectomy can vary depending on the type of procedure and the patient’s individual circumstances. However, in general, most patients can expect to experience some discomfort and swelling for a few days after the procedure.
Patients may need to follow a special diet or avoid certain activities for a period of time after the procedure. Your dentist or oral surgeon will provide specific instructions on how to care for the surgical site and what to expect during the recovery period.
Is Medicaid Coverage Better or Worse than Private Insurance?
In today’s world, where medical procedures and treatments are becoming more advanced and sophisticated, individuals with oral health issues are often left wondering if their insurance covers these procedures. One of the most common concerns is whether Medicaid covers frenectomy, a procedure that can help individuals with tongue-tie or lip-tie issues. The answer is not as straightforward as one might think, but with a little research, one can find out if their Medicaid plan covers this procedure.
Medicaid coverage for frenectomy varies from state to state. While some states offer coverage for the procedure, others do not. In states where it is covered, there may be certain limitations and restrictions on who is eligible for the procedure. It’s important to consult with your dentist or oral surgeon and your Medicaid plan to determine if you are eligible for coverage. With the right information, you can make an informed decision about your oral health and get the treatment you need.
Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering individuals to make well-informed decisions. Guided by his passion, he has assembled a team of seasoned insurance professionals committed to simplifying the intricate world of insurance for you.
- Latest Posts by Rakibul Hasan
-
Can I Keep Medicaid If My Job Offers Insurance?
- -
Does Smile Direct Club Take Medicaid Insurance?
- -
Does Life Insurance Payout Affect Medicaid?
- All Posts
