Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering...Read more
As we age, our bodies may develop pain and discomfort that can hinder our daily activities. This is especially true for individuals suffering from joint pain, arthritis, and other musculoskeletal conditions. While there are various treatment options available, prolotherapy has been gaining popularity as a non-surgical alternative that can provide long-lasting relief. However, the cost of prolotherapy treatment can be a concern for many, leading them to wonder if Medicare covers this type of therapy.
In this article, we will explore the ins and outs of Medicare coverage for prolotherapy. We will discuss the conditions that may or may not be covered, the types of Medicare plans that provide coverage, and what to expect when seeking prolotherapy treatment under Medicare. So, if you or a loved one are considering prolotherapy as a treatment option, keep reading to find out everything you need to know about Medicare coverage for this therapy.
Contents
- Does Medicare Cover Prolotherapy?
- Frequently Asked Questions
- Does Medicare Cover Prolotherapy?
- What are the Benefits of Prolotherapy?
- Is Prolotherapy Covered by Private Insurance?
- How Many Prolotherapy Treatments are Needed?
- What is the Cost of Prolotherapy?
- GREAT NEWS – Medicare Covers Regenerative Medicine Injections For Arthritis!
- Can I Keep Medicaid If My Job Offers Insurance?
- Does Smile Direct Club Take Medicaid Insurance?
- Does Life Insurance Payout Affect Medicaid?
Does Medicare Cover Prolotherapy?
Prolotherapy has gained popularity in recent years as a non-surgical treatment option for chronic pain. But despite its benefits, many patients are left wondering if their Medicare insurance plan will cover the cost of this treatment. In this article, we’ll explore whether Medicare covers prolotherapy and what patients need to know.
What is Prolotherapy?
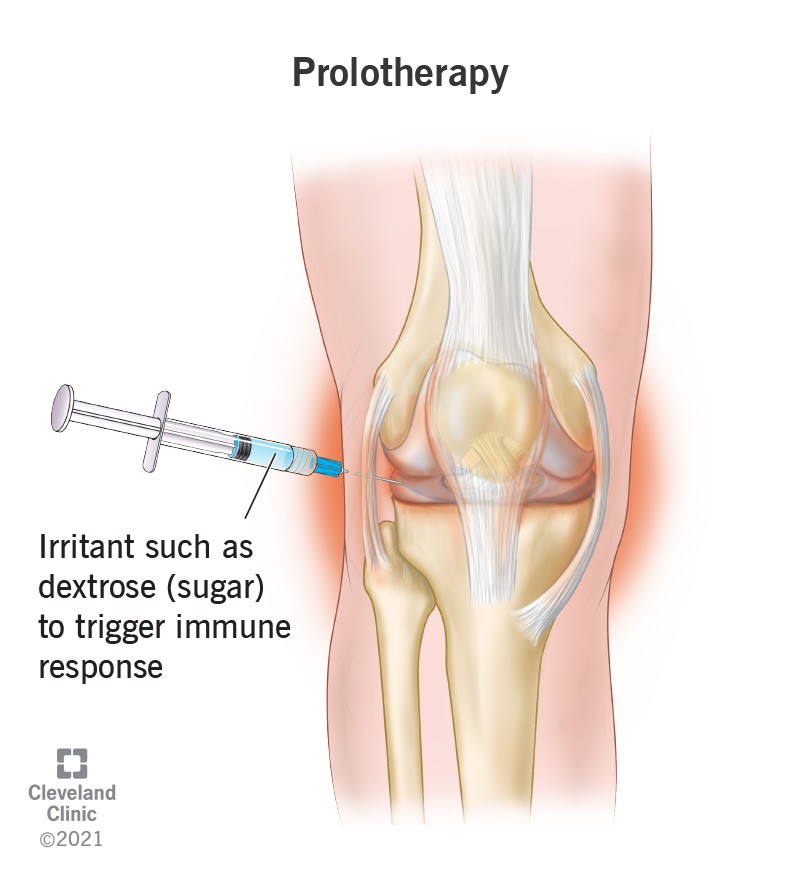
Prolotherapy, also known as regenerative injection therapy, is a non-surgical treatment that involves injecting a solution into damaged or injured tissue to stimulate the body’s natural healing process. The solution, typically a mixture of dextrose and lidocaine, creates a localized inflammation that triggers the body’s immune system to repair the damaged tissue.
Prolotherapy is commonly used to treat chronic pain caused by conditions such as arthritis, tendonitis, and joint instability. It can be used on various parts of the body, including the neck, back, knees, and shoulders.
Does Medicare Cover Prolotherapy?
The answer to this question is not straightforward. Medicare does cover some forms of prolotherapy, but not all. Whether or not Medicare covers prolotherapy depends on the specific type of prolotherapy being used.
Medicare will cover prolotherapy if it is deemed medically necessary and is used to treat a condition that is covered by Medicare. For example, if prolotherapy is used to treat knee osteoarthritis, which is a covered condition, Medicare may cover the cost of the treatment.
However, if prolotherapy is used for non-covered conditions or is considered experimental or investigational, Medicare will not cover the cost of the treatment.
Types of Prolotherapy Covered by Medicare
Medicare covers two types of prolotherapy: prolotherapy with dextrose and prolotherapy with platelet-rich plasma (PRP).
Prolotherapy with dextrose involves injecting a solution of dextrose and lidocaine into the affected area to stimulate the body’s natural healing process. This type of prolotherapy is covered by Medicare when it is deemed medically necessary and used to treat a covered condition.
Prolotherapy with PRP involves injecting a solution of the patient’s own platelet-rich plasma into the affected area to promote healing. Medicare will cover the cost of PRP prolotherapy when it is used to treat chronic non-healing wounds, such as diabetic foot ulcers.
Benefits of Prolotherapy
Prolotherapy has several benefits that make it an attractive treatment option for patients suffering from chronic pain. Some of the benefits of prolotherapy include:
- Non-surgical treatment option
- No downtime or recovery period
- Relieves pain and improves function
- Stimulates the body’s natural healing process
- Low risk of complications
Prolotherapy vs. Surgery
Prolotherapy is often used as an alternative to surgery for patients with chronic pain. While surgery may be necessary in some cases, prolotherapy offers several advantages over surgery. Prolotherapy is a non-surgical treatment that does not require anesthesia or a hospital stay, and there is no downtime or recovery period. Prolotherapy also carries a lower risk of complications than surgery.
However, there are some cases where surgery may be the better option. Patients with severe or advanced cases of arthritis or joint damage may require surgery to repair the damage.
Conclusion
Prolotherapy is a non-surgical treatment option that can provide relief for patients suffering from chronic pain. While Medicare does cover some forms of prolotherapy, it is important for patients to understand what is and is not covered by their insurance plan. Patients should speak with their healthcare provider and insurance provider to determine if prolotherapy is a covered treatment option for their specific condition.
Frequently Asked Questions
Does Medicare Cover Prolotherapy?
Prolotherapy is a medical procedure that involves injecting a solution into the affected area to stimulate healing. It is often used to treat chronic pain and joint injuries. While some private insurance plans may cover prolotherapy, Medicare does not typically cover this procedure.
However, there are some exceptions to this rule. In some cases, Medicare may cover prolotherapy if it is deemed medically necessary and meets certain criteria. For example, if a patient has a joint injury that has not responded to conservative treatments such as physical therapy, medication, and rest, Medicare may consider covering prolotherapy.
What are the Benefits of Prolotherapy?
Prolotherapy has been shown to be an effective treatment for chronic pain and joint injuries. It works by stimulating the body’s natural healing process, which can help reduce pain and inflammation in the affected area. Unlike surgery, prolotherapy is a minimally invasive procedure that does not require a lengthy recovery time.
Additionally, prolotherapy is a safe and non-toxic treatment option that does not carry the same risks as other treatments such as steroid injections or surgery. It can also be used to treat a wide range of conditions, including arthritis, back pain, and sports injuries.
Is Prolotherapy Covered by Private Insurance?
Whether or not prolotherapy is covered by private insurance depends on the specific policy. Some insurance plans may cover prolotherapy as a form of treatment for chronic pain and joint injuries. However, other plans may have restrictions or require pre-authorization before covering the procedure.
It is important to check with your insurance provider to determine if prolotherapy is covered under your plan. You may also want to consult with your healthcare provider to discuss alternative treatment options if prolotherapy is not covered by your insurance.
How Many Prolotherapy Treatments are Needed?
The number of prolotherapy treatments needed depends on the individual and the specific condition being treated. In general, most patients require a series of treatments spaced several weeks apart to achieve optimal results.
Your healthcare provider will work with you to develop a treatment plan that is tailored to your individual needs. This may include a combination of prolotherapy, physical therapy, and other treatments to help manage your pain and improve your overall health and well-being.
What is the Cost of Prolotherapy?
The cost of prolotherapy can vary depending on several factors, including the location of the treatment, the provider, and the number of treatments needed. In general, prolotherapy is a relatively affordable treatment option compared to other treatments such as surgery or long-term medication use.
If you are considering prolotherapy, it is important to check with your insurance provider to determine if the procedure is covered under your plan. You may also want to consult with your healthcare provider to discuss alternative treatment options if cost is a concern.
GREAT NEWS – Medicare Covers Regenerative Medicine Injections For Arthritis!
In conclusion, Medicare coverage for prolotherapy may not be straightforward, but it is possible to receive coverage under certain circumstances. As a professional writer, it is important to understand the intricacies of Medicare coverage and the potential benefits of prolotherapy for those suffering from chronic pain. By working with healthcare providers and insurance companies, patients can explore their options and make informed decisions about their treatment plans.
Ultimately, the decision to pursue prolotherapy as a treatment option should be based on individual needs and preferences, as well as the advice of medical professionals. While Medicare coverage may vary, it is important to consider the potential benefits of prolotherapy for reducing pain and improving overall quality of life. As a professional writer, it is crucial to stay informed about healthcare trends and developments, and to advocate for access to innovative treatments that can make a difference in the lives of patients.
Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering individuals to make well-informed decisions. Guided by his passion, he has assembled a team of seasoned insurance professionals committed to simplifying the intricate world of insurance for you.
- Latest Posts by Rakibul Hasan
-
Can I Keep Medicaid If My Job Offers Insurance?
- -
Does Smile Direct Club Take Medicaid Insurance?
- -
Does Life Insurance Payout Affect Medicaid?
- All Posts