Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering...Read more
When it comes to seeking medical treatment, one of the most important factors to consider is the cost. For individuals who are covered by Medicare, this is especially true. Many people wonder how many transcranial magnetic stimulation (TMS) treatments Medicare will cover, as this innovative treatment has been proven to be effective for a range of mental health conditions.
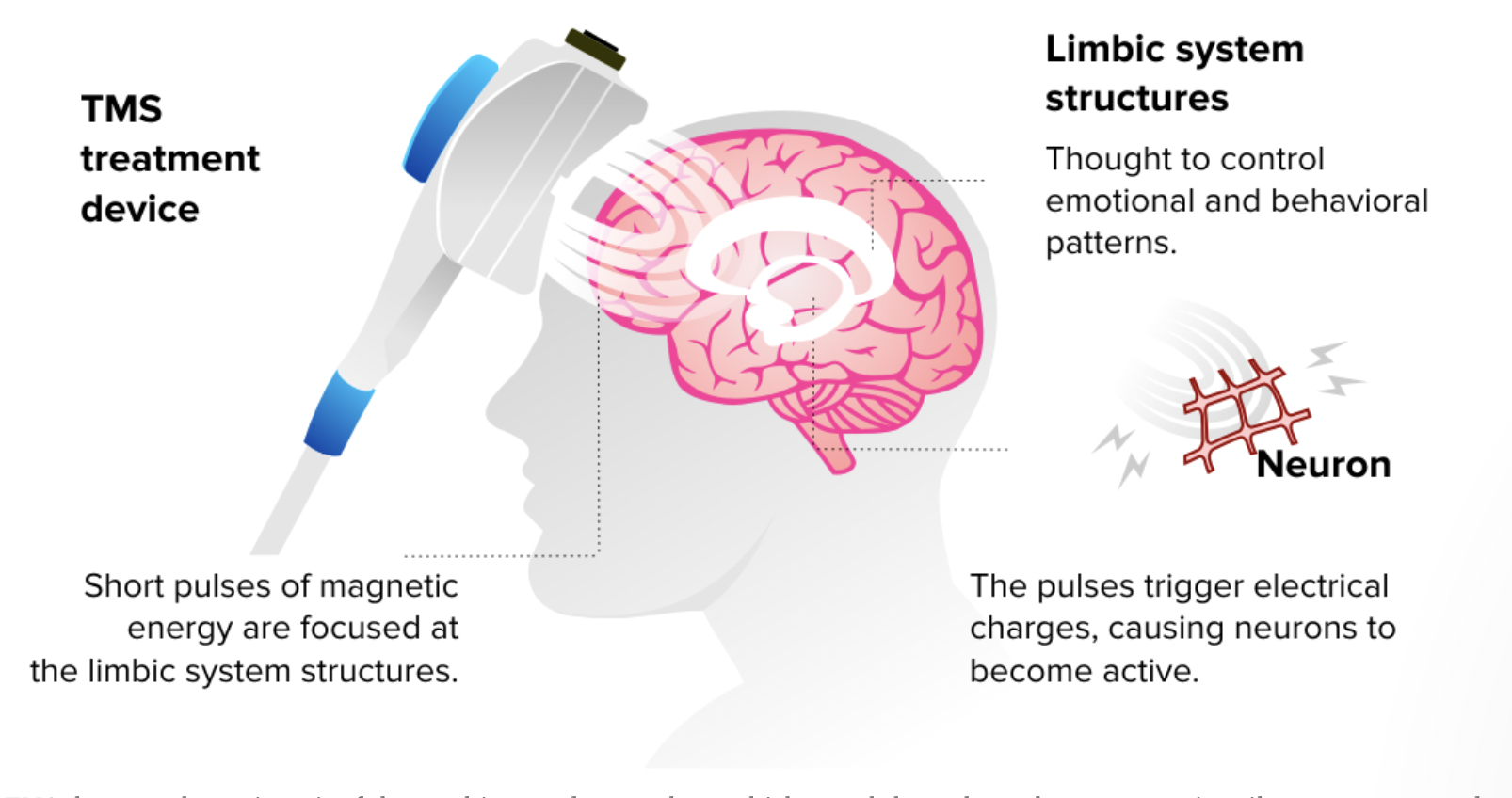
TMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. It has been approved by the FDA for the treatment of depression, and has also shown promise for anxiety, PTSD, and other conditions. However, the cost of these treatments can be significant, and many patients are concerned about whether Medicare will cover the cost. In this article, we will explore the details of Medicare coverage for TMS treatments, and provide helpful information for those who may be considering this treatment option.
Medicare covers TMS (Transcranial Magnetic Stimulation) treatments for major depressive disorder. Typically, Medicare covers up to 36 TMS treatments over 12 weeks. However, the number of treatments covered by Medicare may vary depending on the individual’s medical condition and the medical necessity of the treatment. It is always best to consult with a healthcare provider and Medicare to determine the coverage for TMS treatments.
How Many Tms Treatments Does Medicare Cover?
Transcranial Magnetic Stimulation (TMS) therapy is a form of treatment for depression and other mental health disorders. TMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. Medicare is a federal health insurance program that covers TMS therapy for certain individuals. But, how many TMS treatments does Medicare cover? Let’s explore this in detail.
What is TMS Therapy?
Transcranial Magnetic Stimulation (TMS) therapy is an FDA approved treatment for depression and other mental health disorders. TMS therapy is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. The treatment involves placing an electromagnetic coil against the scalp, which delivers a magnetic pulse to the brain. The magnetic pulse stimulates the nerve cells in the brain that are responsible for regulating mood.
TMS therapy is an effective treatment for depression, especially for individuals who have not responded well to other treatments. The therapy has no systemic side effects and is well-tolerated by patients. TMS therapy is also used to treat other mental health disorders, such as anxiety, bipolar disorder, and PTSD.
Does Medicare Cover TMS Therapy?
Yes, Medicare covers TMS therapy for certain individuals. Medicare covers TMS therapy for individuals who have been diagnosed with treatment-resistant depression. Treatment-resistant depression is defined as depression that has not responded to at least four different antidepressant medications.
Medicare covers TMS therapy as an outpatient procedure, which means that the treatment is not covered if it is performed in a hospital. Medicare covers TMS therapy for up to 36 sessions over a nine-week period. The number of sessions may be extended if the patient has not responded to the initial treatment.
What are the Benefits of TMS Therapy?
TMS therapy has several benefits over traditional treatments for depression. The therapy is non-invasive and does not require anesthesia or sedation. TMS therapy does not have systemic side effects, such as weight gain or sexual dysfunction, which are common with antidepressant medications.
TMS therapy is also effective for individuals who have not responded well to other treatments. The therapy has been shown to improve mood and reduce symptoms of depression in individuals who have not responded to antidepressant medications.
TMS Therapy vs. Electroconvulsive Therapy (ECT)
Electroconvulsive Therapy (ECT) is another form of treatment for depression that is covered by Medicare. ECT is a more invasive procedure that involves sending an electrical current through the brain to induce a seizure. ECT is typically used for individuals with severe depression who have not responded to other treatments.
TMS therapy is a less invasive alternative to ECT. TMS therapy does not have the same side effects as ECT, such as memory loss and confusion. TMS therapy is also more convenient for patients, as it does not require hospitalization.
Conclusion
TMS therapy is an effective treatment for depression and other mental health disorders. Medicare covers TMS therapy for individuals who have been diagnosed with treatment-resistant depression. The therapy is non-invasive and does not have systemic side effects. TMS therapy is a less invasive alternative to ECT and is more convenient for patients. If you or a loved one has been diagnosed with treatment-resistant depression, talk to your doctor about TMS therapy and whether it is covered by Medicare.
Contents
- Frequently Asked Questions
- What is TMS treatment, and how does it work?
- Does Medicare cover TMS treatment?
- How many TMS treatments does Medicare cover?
- Do I need to meet any criteria to be eligible for TMS treatment under Medicare?
- How do I find a healthcare provider who offers TMS treatment under Medicare?
- How Much Does TMS Cost? Is TMS Covered by Insurance?
- Can I Keep Medicaid If My Job Offers Insurance?
- Does Smile Direct Club Take Medicaid Insurance?
- Does Life Insurance Payout Affect Medicaid?
Frequently Asked Questions
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure used to treat depression. It involves the use of electromagnetic pulses to stimulate nerve cells in the brain. Medicare is a federal health insurance program that covers TMS treatment for eligible individuals. Here are some common questions about TMS treatment and Medicare coverage.
What is TMS treatment, and how does it work?
TMS treatment is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. The procedure involves placing a magnetic coil against the scalp, which produces electromagnetic pulses that stimulate nerve cells in the brain. This stimulation is thought to alleviate symptoms of depression by increasing activity in certain areas of the brain.
TMS treatment is typically used for individuals who have not responded to traditional treatments for depression, such as medication or psychotherapy. It is generally considered safe and well-tolerated, with few side effects.
Does Medicare cover TMS treatment?
Yes, Medicare covers TMS treatment for eligible individuals. However, coverage may vary depending on the specific plan and the individual’s circumstances. In general, Medicare covers TMS treatment for individuals who have been diagnosed with major depression and who have not responded to traditional treatments.
Before receiving TMS treatment, it is important to check with Medicare to determine coverage and any out-of-pocket costs that may be associated with the procedure.
How many TMS treatments does Medicare cover?
The number of TMS treatments that Medicare covers can vary depending on the individual’s circumstances. In general, Medicare covers up to 36 TMS treatments for individuals with major depression who have not responded to traditional treatments.
However, the number of treatments covered may be subject to review and may vary depending on the individual’s specific plan and medical history.
Do I need to meet any criteria to be eligible for TMS treatment under Medicare?
Yes, to be eligible for TMS treatment under Medicare, you must meet certain criteria. First, you must have been diagnosed with major depression by a qualified healthcare provider. Additionally, you must have tried and failed to respond to traditional treatments, such as medication or psychotherapy.
Finally, you must meet certain medical criteria to ensure that TMS treatment is safe and appropriate for you. Your healthcare provider can help you determine if you meet these criteria and if TMS treatment is the right option for you.
How do I find a healthcare provider who offers TMS treatment under Medicare?
To find a healthcare provider who offers TMS treatment under Medicare, you can start by contacting Medicare directly. They can provide you with a list of providers in your area who offer TMS treatment and can help you determine your eligibility for coverage.
You can also ask your healthcare provider for a referral or search online for providers in your area who offer TMS treatment under Medicare.
How Much Does TMS Cost? Is TMS Covered by Insurance?
As we age, it’s natural for our bodies to experience wear and tear, which can lead to chronic pain and a host of other ailments. For many seniors, Transcranial Magnetic Stimulation (TMS) therapy has been a game-changer, offering a non-invasive, drug-free alternative to conventional treatments. But the big question on everyone’s mind is, “How many TMS treatments does Medicare cover?”
The answer is that Medicare covers TMS therapy for patients with Major Depressive Disorder who have not responded to at least one antidepressant medication. The number of treatments covered depends on the individual’s response to therapy, with most patients receiving between 20-30 treatments. While Medicare coverage varies depending on the state and provider, it’s important to note that TMS therapy is covered under Medicare Part B, which typically pays for 80% of the cost after the deductible is met.
In conclusion, TMS therapy is a promising option for seniors dealing with depression, anxiety, and other mental health conditions. While Medicare coverage can vary, it’s important for patients to discuss their options with their healthcare providers and insurance carriers to determine the best course of treatment. With proper care and attention, TMS therapy can provide relief and improve quality of life for those in need.
Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering individuals to make well-informed decisions. Guided by his passion, he has assembled a team of seasoned insurance professionals committed to simplifying the intricate world of insurance for you.
- Latest Posts by Rakibul Hasan
-
Can I Keep Medicaid If My Job Offers Insurance?
- -
Does Smile Direct Club Take Medicaid Insurance?
- -
Does Life Insurance Payout Affect Medicaid?
- All Posts
