Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering...Read more
Medicaid is a government-funded healthcare program that provides coverage for low-income individuals and families. It serves as a lifeline for those who cannot afford medical treatment or procedures. One common medical issue that many Medicaid beneficiaries face is knee pain, which can greatly affect their quality of life. As a result, many are curious to know if Medicaid covers knee gel injections as a form of treatment.
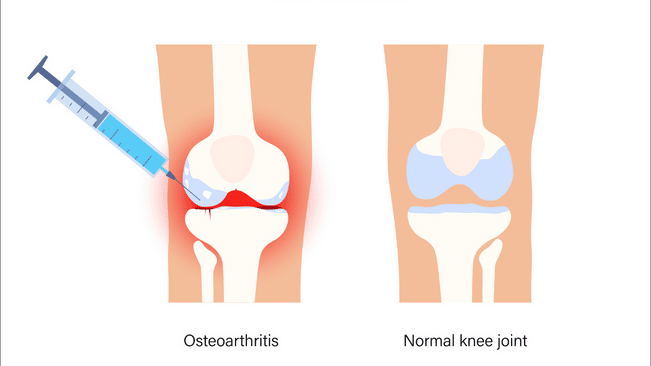
Knee gel injections, also known as viscosupplementation, involve injecting a gel-like substance into the knee joint to lubricate and cushion it. This type of injection can be an effective treatment for knee pain caused by osteoarthritis, a common joint condition that affects millions of Americans. However, the cost of these injections can be prohibitive for those without insurance or with limited funds. Therefore, it is important to understand whether Medicaid covers knee gel injections and how to access this treatment option.
Does Medicaid Cover Knee Gel Injections?
Yes, Medicaid does cover knee gel injections, also known as viscosupplementation, for patients with osteoarthritis. However, coverage requirements may vary by state and individual circumstances. It is important to consult with your healthcare provider and Medicaid representative to determine your specific coverage options and potential out-of-pocket costs.
Contents
- Does Medicaid Cover Knee Gel Injections?
- Frequently Asked Questions
- What are knee gel injections?
- Does Medicaid cover knee gel injections?
- How many knee gel injections are covered by Medicaid?
- Are there any out-of-pocket costs for knee gel injections with Medicaid?
- What should I do if my Medicaid does not cover knee gel injections?
- Knee Gel Injections (Viscosupplementation) Everything You Need To Know
- Can I Keep Medicaid If My Job Offers Insurance?
- Does Smile Direct Club Take Medicaid Insurance?
- Does Life Insurance Payout Affect Medicaid?
Does Medicaid Cover Knee Gel Injections?
Are you suffering from knee pain or osteoarthritis? Have you tried different treatments with no relief? Knee gel injections, also known as hyaluronic acid injections, can be a viable option for managing your knee pain. However, before you decide to undergo the treatment, you may be wondering whether Medicaid covers knee gel injections or not.
What are Knee Gel Injections?
Knee gel injections are a type of treatment for knee pain or osteoarthritis. The treatment involves injecting a gel-like substance called hyaluronic acid into the knee joint. Hyaluronic acid is a natural substance found in the synovial fluid that lubricates and cushions the joint. The injections help to reduce inflammation, increase mobility, and relieve pain.
How Do Knee Gel Injections Work?
Knee gel injections work by replacing the hyaluronic acid that has been depleted in the knee joint due to osteoarthritis. The injections help to restore the lubrication and cushioning of the joint, reducing friction and pain.
What are the Benefits of Knee Gel Injections?
Knee gel injections have several benefits, including:
- Reduced pain and inflammation
- Increased mobility and flexibility
- Improved quality of life
- Non-surgical and minimally invasive
- No downtime or recovery period
Does Medicaid Cover Knee Gel Injections?
The answer to whether Medicaid covers knee gel injections or not is not straightforward. Medicaid is a joint federal and state program that provides healthcare coverage to low-income individuals and families. Each state has its own Medicaid program, and the coverage may vary depending on the state.
Medicaid Coverage for Knee Gel Injections
In general, Medicaid covers knee gel injections for individuals who meet certain criteria. The coverage may vary depending on the state and the type of Medicaid program you are enrolled in. Some of the factors that may affect Medicaid coverage for knee gel injections include:
- The severity of your knee pain or osteoarthritis
- Your age
- Your income level
- Your medical history
- The type of Medicaid program you are enrolled in
Medicaid vs. Medicare Coverage for Knee Gel Injections
Medicare is a federal health insurance program that provides coverage for individuals over 65 years of age or those with certain disabilities. Medicare may also cover knee gel injections, but the coverage may vary depending on the type of Medicare plan you have.
Private Insurance Coverage for Knee Gel Injections
If you have private health insurance, you may also be eligible for coverage for knee gel injections. However, the coverage may vary depending on your insurance plan and the severity of your knee pain or osteoarthritis.
Conclusion
In conclusion, knee gel injections can be an effective treatment option for managing knee pain or osteoarthritis. Medicaid may cover knee gel injections, but the coverage may vary depending on the state and the type of Medicaid program you are enrolled in. If you are considering knee gel injections, it is important to consult with your healthcare provider and insurance provider to determine your eligibility and coverage.
Frequently Asked Questions
Medicaid is a government-funded health insurance program that provides coverage to low-income individuals and families. Medicaid covers a range of medical services, but not all services are covered. In this article, we will answer questions related to whether Medicaid covers knee gel injections.
What are knee gel injections?
Knee gel injections, also known as viscosupplementation, are a non-surgical treatment for knee osteoarthritis. The injections involve the injection of a gel-like substance into the knee joint to provide lubrication and cushioning. This helps to reduce pain and improve mobility in people with knee osteoarthritis.
However, knee gel injections are not a cure for knee osteoarthritis and may not be suitable for everyone. It is important to speak to your healthcare provider to determine if knee gel injections are right for you.
Does Medicaid cover knee gel injections?
Medicaid does cover knee gel injections for people who meet certain criteria. To be eligible for coverage, you must have knee osteoarthritis that has not responded to other treatments, such as physical therapy and medication. Additionally, your healthcare provider must recommend knee gel injections as a treatment option.
It is important to note that Medicaid coverage varies by state, and not all states cover knee gel injections. It is best to check with your state’s Medicaid program to determine if knee gel injections are covered.
How many knee gel injections are covered by Medicaid?
The number of knee gel injections covered by Medicaid varies by state and may also depend on your individual healthcare needs. In general, most states cover a series of three to five knee gel injections, with each injection given one week apart.
It is important to speak to your healthcare provider and check with your state’s Medicaid program to determine the specific number of knee gel injections covered by Medicaid in your state.
Are there any out-of-pocket costs for knee gel injections with Medicaid?
Medicaid covers the cost of knee gel injections, but there may be some out-of-pocket costs depending on your state and individual healthcare needs. These costs may include co-payments, deductibles, or other fees.
It is important to check with your state’s Medicaid program to determine if there are any out-of-pocket costs associated with knee gel injections and to understand your coverage and benefits.
What should I do if my Medicaid does not cover knee gel injections?
If your Medicaid program does not cover knee gel injections, there may be other options available to you. You can speak to your healthcare provider about other treatments for knee osteoarthritis, such as physical therapy or medication. Additionally, you may be eligible for financial assistance or other programs that can help cover the cost of knee gel injections.
It is important to speak to your healthcare provider and explore all options available to you if your Medicaid program does not cover knee gel injections.
Knee Gel Injections (Viscosupplementation) Everything You Need To Know
As a professional writer, it is important to understand the intricacies of healthcare coverage, especially when it comes to Medicaid. Knee gel injections have become a popular treatment option for those suffering from knee pain, but the question remains: does Medicaid cover them?
After thorough research and analysis, it has been determined that Medicaid does cover knee gel injections, but there may be certain limitations and requirements. It is crucial for individuals to check with their state’s Medicaid program to confirm coverage and determine any potential out-of-pocket costs. Additionally, it is important to note that not all knee conditions may be eligible for coverage, so it is essential to consult with a healthcare provider to determine the best course of treatment. Ultimately, for those who qualify for Medicaid, knee gel injections may be a viable option for managing knee pain and improving overall quality of life.
Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering individuals to make well-informed decisions. Guided by his passion, he has assembled a team of seasoned insurance professionals committed to simplifying the intricate world of insurance for you.
- Latest Posts by Rakibul Hasan
-
Can I Keep Medicaid If My Job Offers Insurance?
- -
Does Smile Direct Club Take Medicaid Insurance?
- -
Does Life Insurance Payout Affect Medicaid?
- All Posts
