Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering...Read more
As we age, it is not uncommon to require medical care and attention that goes beyond a hospital stay. This is where swing beds come in handy. Swing beds are a type of transitional care that allows patients to receive medical care in a hospital setting without the need for acute care. But how long does Medicare pay for swing beds, and what factors determine the duration of coverage?
If you or a loved one require the use of a swing bed, it is important to understand how long Medicare covers the cost. Medicare is a federal health insurance program that provides coverage to individuals who are 65 years or older, have certain disabilities, or have end-stage renal disease. While Medicare does cover swing beds, the duration of coverage depends on several factors, including the patient’s condition and the level of care required. In this article, we will explore the ins and outs of Medicare coverage for swing beds and what patients and caregivers need to know.
How Long Does Medicare Pay for Swing Bed?
If you or your loved one is in need of extended care after a hospital stay, Medicare may cover the cost of a swing bed. A swing bed is a hospital bed that can be used for either acute or skilled care. Medicare covers the cost of swing bed care for a limited time, but how long does Medicare pay for swing bed care? In this article, we will explore the answer to this question and other important details about Medicare coverage for swing beds.
What is a Swing Bed?
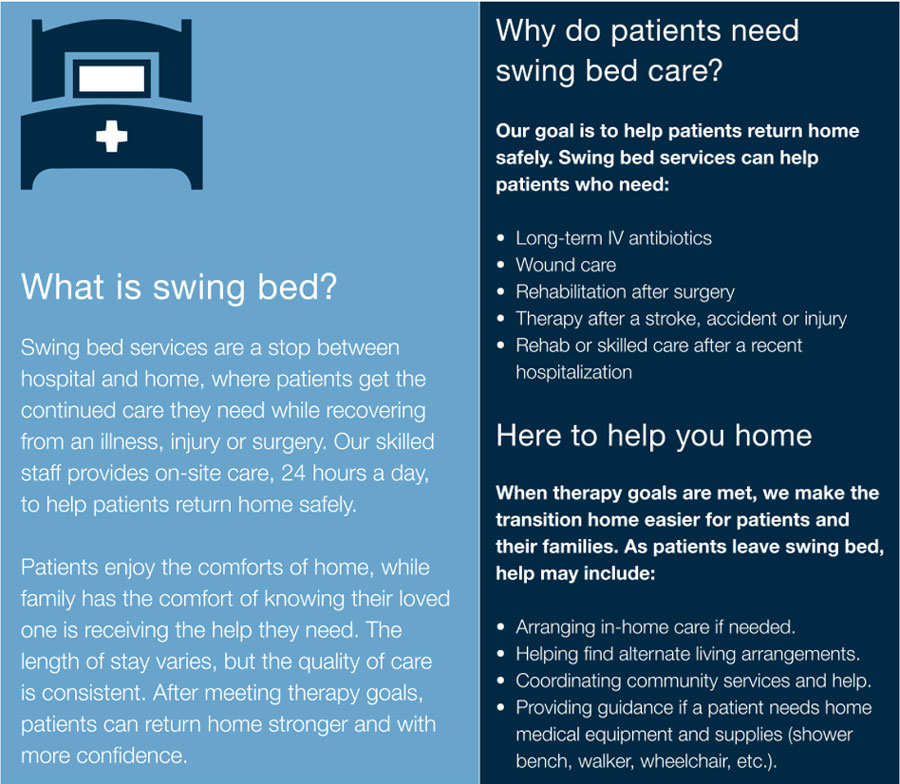
A swing bed is a hospital bed that can be used for either acute or skilled care. This bed is located in a hospital or skilled nursing facility and can be used for patients who no longer need acute care but still require daily medical attention. Patients who need rehabilitation, wound care, or other types of skilled care can receive this care in a swing bed.
Acute Care vs. Skilled Care
Acute care is medical treatment for a sudden illness or injury that requires immediate attention. Skilled care is a type of medical care that is provided by trained medical professionals such as physical therapists, occupational therapists, or speech therapists. Examples of skilled care include wound care, rehabilitation, and intravenous therapy.
What Does Medicare Cover?
Medicare Part A covers the cost of a swing bed if the patient meets certain criteria. The patient must have been hospitalized for at least three consecutive days for an acute illness or injury, and the swing bed must be in the same hospital or a skilled nursing facility that has a Medicare certification. Medicare will cover up to 100 days of swing bed care per benefit period.
What Happens After 100 Days?
After 100 days of swing bed care, Medicare coverage will end. If the patient still requires skilled care, they may be eligible for coverage under another Medicare benefit such as home health care or hospice care. If the patient requires long-term care, they may need to pay for this care out of pocket or with the help of other insurance coverage.
Benefits of Swing Bed Care
Swing bed care can provide several benefits to patients who need extended care after a hospital stay. Some of these benefits include:
- Access to skilled medical professionals such as physical therapists, occupational therapists, and speech therapists
- Continued medical care and monitoring
- Wound care and medication management
- Rehabilitation services to help regain strength and mobility
- Transition to home health care or hospice care if needed
Swing Bed Care vs. Nursing Home Care
Swing bed care and nursing home care are both options for patients who need extended medical care. However, there are some differences between the two. Swing bed care is provided in a hospital or skilled nursing facility and is intended for patients who no longer need acute care but still require daily medical attention. Nursing home care is provided in a long-term care facility and is intended for patients who require ongoing medical care and assistance with daily living activities.
Which Option is Right for You?
The decision between swing bed care and nursing home care will depend on the individual patient’s needs and preferences. Patients who require ongoing medical care and assistance with daily living activities may be better suited for nursing home care, while patients who need rehabilitation and skilled care may benefit from swing bed care.
Conclusion
Medicare covers the cost of swing bed care for up to 100 days per benefit period. Swing bed care can provide several benefits to patients who need extended care after a hospital stay, including access to skilled medical professionals and continued medical care and monitoring. The decision between swing bed care and nursing home care will depend on the individual patient’s needs and preferences.
Contents
- Frequently Asked Questions
- How long does Medicare pay for swing bed?
- What happens after Medicare coverage ends?
- Can I switch swing bed facilities during Medicare coverage?
- What is the cost-sharing for swing bed services?
- What happens if I exceed the 100-day limit for swing bed services?
- CMS CAH Swing Bed Requirements and Changes 2022
- Can I Keep Medicaid If My Job Offers Insurance?
- Does Smile Direct Club Take Medicaid Insurance?
- Does Life Insurance Payout Affect Medicaid?
Frequently Asked Questions
Swing bed services are offered by hospitals to patients who have various medical needs. Medicare can cover the cost of these services for a limited time. If you or your loved one needs swing bed services, here are some questions you might have about the duration of Medicare coverage.
How long does Medicare pay for swing bed?
Medicare Part A can pay for swing bed services for up to 20 days. However, if you need more time in swing bed, Medicare may cover some of the cost for days 21-100. To qualify for extended coverage, you must meet certain conditions:
First, you must have been admitted to the hospital for at least three consecutive days. The swing bed services that you receive must also be related to the condition or illness that caused your hospitalization. Additionally, your doctor must certify that you need daily skilled care that can only be provided in a swing bed facility. If you meet these criteria, Medicare can cover up to 80% of the cost for days 21-100.
What happens after Medicare coverage ends?
After Medicare coverage for swing bed services ends, you will be responsible for paying any remaining costs. These costs can vary depending on your insurance coverage and the specific swing bed facility that you use. You should also consider other options for ongoing care, such as home health services or long-term care facilities.
If you are unable to pay for swing bed services out of pocket, you may be able to qualify for Medicaid or other assistance programs. Speak with a social worker or financial counselor at your hospital to learn more about your options.
Can I switch swing bed facilities during Medicare coverage?
Yes, you can switch swing bed facilities during Medicare coverage. However, you should be aware that not all facilities may accept Medicare or have available beds. You should also consider the distance from your home and the quality of care provided by the facility when choosing a new location.
Before switching facilities, you should speak with your doctor and care team to ensure that the new facility can meet your medical needs. You should also coordinate with the new facility and your insurance provider to ensure that Medicare coverage will continue without interruption.
What is the cost-sharing for swing bed services?
For days 1-20, Medicare Part A covers the full cost of swing bed services. However, for days 21-100, you will be responsible for a daily coinsurance amount. In 2021, this coinsurance amount is $185.50 per day. Some Medicare Supplement Insurance plans may cover this coinsurance amount, so be sure to check your policy details.
If you do not have insurance coverage for the coinsurance amount, you will be responsible for paying it out of pocket. However, if you are unable to pay, you may be able to qualify for financial assistance or payment plans through the swing bed facility or other programs.
What happens if I exceed the 100-day limit for swing bed services?
If you exceed the 100-day limit for swing bed services, Medicare will no longer cover the cost of your care. You will be responsible for paying the full cost of your care from that point forward.
If you need ongoing care, you should consider other options such as home health services or long-term care facilities. Speak with your doctor and care team to determine the best plan for your ongoing care needs.
CMS CAH Swing Bed Requirements and Changes 2022
As a professional writer, I understand the importance of providing a comprehensive answer to the question of how long Medicare pays for swing bed services. Generally, Medicare pays for swing bed services for up to 100 days, provided the patient has met certain eligibility criteria. This coverage is available to patients who have been discharged from a hospital after a three-night stay and require skilled nursing care for their condition.
It is important to note that Medicare pays for swing bed services on a limited basis, and patients are responsible for any additional costs beyond the 100-day coverage period. Additionally, patients must meet certain conditions to continue receiving coverage, such as requiring daily skilled nursing care and showing progress towards their recovery goals. As a professional writer, I hope this information provides clarity for those seeking information on Medicare coverage for swing bed services and encourages patients to explore all available options for their healthcare needs.
Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering individuals to make well-informed decisions. Guided by his passion, he has assembled a team of seasoned insurance professionals committed to simplifying the intricate world of insurance for you.
- Latest Posts by Rakibul Hasan
-
Can I Keep Medicaid If My Job Offers Insurance?
- -
Does Smile Direct Club Take Medicaid Insurance?
- -
Does Life Insurance Payout Affect Medicaid?
- All Posts
