Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering...Read more
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. It is a promising treatment option for various mental health conditions such as depression, anxiety, and OCD. However, the cost of TMS treatment can be a significant barrier for patients who need it. This has raised the question, “Is Transcranial Magnetic Stimulation covered by Medicare?”
In this article, we will explore the answer to this question and provide you with all the relevant information you need to know about TMS and Medicare coverage. We will delve into the specifics of Medicare’s policies and guidelines on TMS coverage, and discuss what patients can expect when it comes to insurance coverage for this innovative treatment option. So, whether you are a patient considering TMS treatment, or a healthcare provider looking for information on Medicare coverage, keep reading to find out everything you need to know about TMS and Medicare.
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure used to treat depression. Medicare does cover TMS, but only for patients who have tried at least four antidepressant medications without success. Medicare also requires that the TMS treatment is provided by a licensed healthcare provider in an approved facility. Patients will need to meet certain criteria to be eligible for coverage, and out-of-pocket costs may still apply.
Contents
- Is Transcranial Magnetic Stimulation Covered by Medicare?
- Frequently Asked Questions
- Question 1: Is TMS covered by Medicare?
- Question 2: What is the process for getting TMS covered by Medicare?
- Question 3: What are the potential out-of-pocket costs for TMS with Medicare?
- Question 4: Are there any risks associated with TMS treatment?
- Question 5: What should patients expect during TMS treatment?
- How Much Does TMS Cost? Is TMS Covered by Insurance?
- Can I Keep Medicaid If My Job Offers Insurance?
- Does Smile Direct Club Take Medicaid Insurance?
- Does Life Insurance Payout Affect Medicaid?
Is Transcranial Magnetic Stimulation Covered by Medicare?
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure used to treat depression, anxiety, and other mental health conditions. The procedure involves the use of a magnetic field to stimulate nerve cells in the brain. While TMS has been found to be an effective treatment for many patients, the cost of the procedure can be a barrier for some individuals. This leads to the question, is TMS covered by Medicare?
What is Transcranial Magnetic Stimulation?
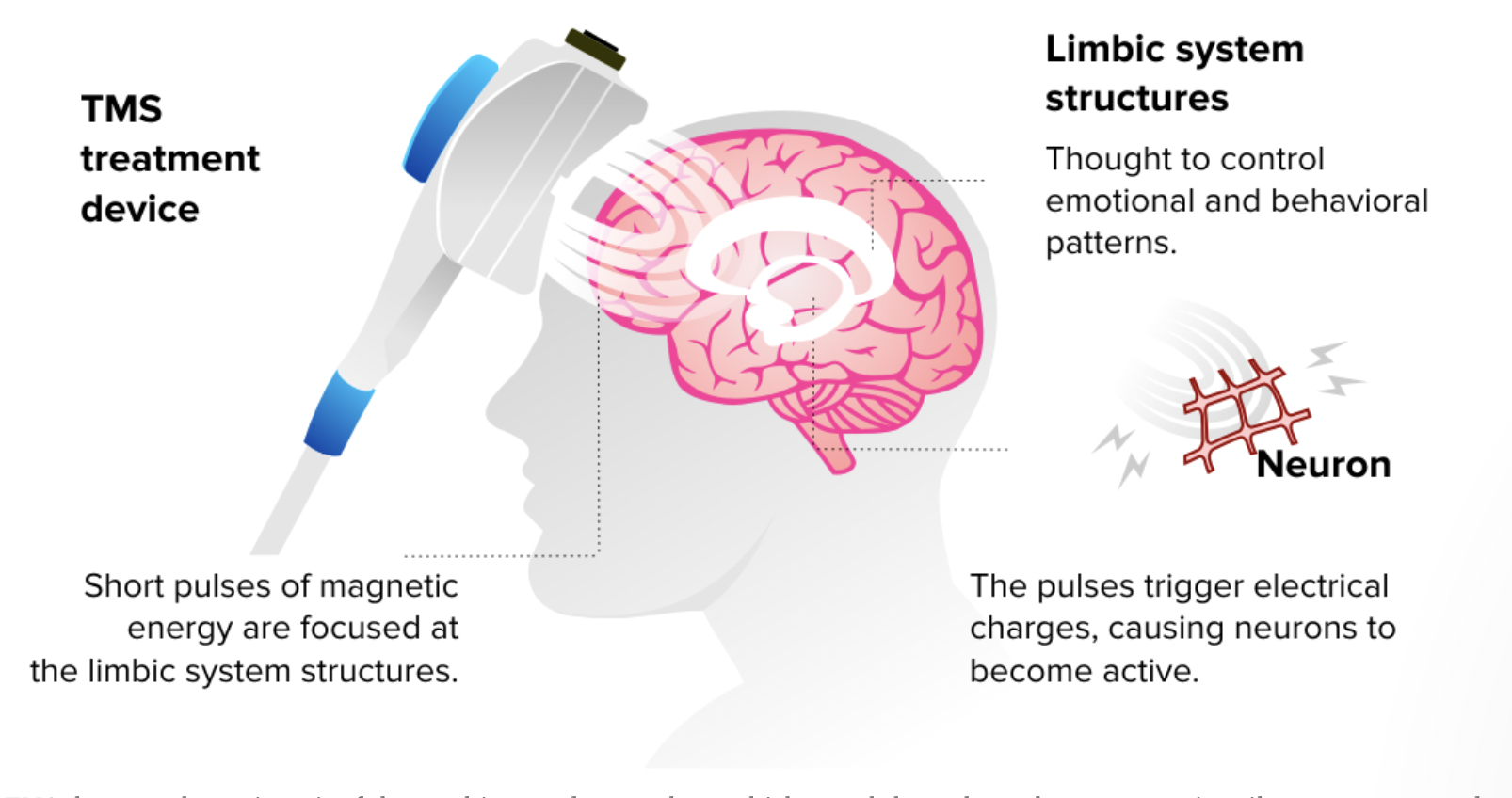
Transcranial Magnetic Stimulation is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. The procedure is typically used to treat depression, anxiety, and other mental health conditions. During the procedure, a coil is placed over the patient’s scalp, and a magnetic field is used to stimulate nerve cells in the brain. The stimulation is believed to improve the communication between different parts of the brain and promote the growth of new brain cells.
How Effective is Transcranial Magnetic Stimulation?
Transcranial Magnetic Stimulation has been found to be an effective treatment for depression, anxiety, and other mental health conditions. Studies have shown that TMS can improve symptoms of depression in up to 50% of patients. The treatment is generally well-tolerated and has few side effects.
Is Transcranial Magnetic Stimulation Covered by Medicare?
The answer to this question is not straightforward. While Medicare does cover some medical procedures, coverage for TMS varies depending on the specific circumstances. Medicare Part B typically covers outpatient mental health services, including TMS. However, Medicare does not cover TMS for all conditions.
Medicare only covers TMS for patients who have tried and failed at least one antidepressant medication. Additionally, the patient must have a diagnosis of Major Depressive Disorder (MDD) and have tried psychotherapy. If these criteria are met, Medicare will cover TMS as a treatment option.
What are the Benefits of Transcranial Magnetic Stimulation?
One of the key benefits of Transcranial Magnetic Stimulation is that it is a non-invasive procedure. Patients do not require anesthesia or sedation, and the procedure is generally well-tolerated. TMS has also been found to have few side effects.
Another benefit of TMS is that it is an effective treatment option for patients who have not responded to traditional treatments like medication and psychotherapy. TMS has been found to improve symptoms of depression in up to 50% of patients who have not responded to other treatments.
Transcranial Magnetic Stimulation vs. Electroconvulsive Therapy
Electroconvulsive Therapy (ECT) is another treatment option for patients with depression and other mental health conditions. ECT involves the use of electrical currents to stimulate the brain. While ECT can be an effective treatment option, it is often associated with side effects like memory loss and confusion.
TMS, on the other hand, is a non-invasive procedure that has few side effects. TMS has been found to be as effective as ECT for the treatment of depression, and it does not carry the same risks associated with ECT.
Conclusion
Transcranial Magnetic Stimulation is a non-invasive procedure used to treat depression, anxiety, and other mental health conditions. While Medicare does cover TMS for certain patients, coverage is not guaranteed. Patients who have not responded to traditional treatments like medication and psychotherapy may benefit from TMS as a treatment option. TMS has been found to be an effective treatment option with few side effects, making it a promising option for many patients.
Frequently Asked Questions
Transcranial Magnetic Stimulation (TMS) is a non-invasive medical procedure that uses magnetic fields to stimulate nerve cells in the brain to treat depression. Many people wonder whether TMS is covered by Medicare or not. Here are some frequently asked questions and their answers about the coverage of TMS by Medicare.
Question 1: Is TMS covered by Medicare?
Yes, Medicare does cover TMS for the treatment of major depressive disorder in patients who have not responded to at least one antidepressant medication. However, Medicare has specific criteria that must be met in order for TMS to be covered. The patient must have a documented diagnosis of major depressive disorder, have tried and failed at least one antidepressant medication, and have a qualifying episode of depression that meets certain severity criteria.
Additionally, the TMS treatment must be administered in a Medicare-approved facility by a healthcare provider who is enrolled in Medicare and meets certain qualifications. The number of TMS treatments covered by Medicare may also be limited to a certain number of sessions.
Question 2: What is the process for getting TMS covered by Medicare?
The process for getting TMS covered by Medicare starts with a visit to a healthcare provider who can evaluate the patient’s depression and determine if TMS is an appropriate treatment option. The provider must document the patient’s diagnosis, treatment history, and the severity of the depression. They will then submit a request for TMS treatment to Medicare for approval.
Once Medicare approves the request, the patient can begin TMS treatment at a Medicare-approved facility. The provider will need to submit documentation of the treatment and the patient’s progress to Medicare for continued coverage.
Question 3: What are the potential out-of-pocket costs for TMS with Medicare?
Medicare covers a portion of the costs of TMS treatment, but there may still be out-of-pocket expenses for the patient. The patient may be responsible for the deductible, coinsurance, and copayment amounts for TMS treatment. These amounts will depend on the type of Medicare plan the patient has and the specific details of their coverage.
It is important for patients to check with their Medicare plan to understand their specific out-of-pocket costs for TMS treatment. Some facilities may also offer financial assistance or payment plans to help with the costs of TMS treatment.
Question 4: Are there any risks associated with TMS treatment?
TMS is generally considered a safe and well-tolerated treatment for depression. The most common side effects of TMS are mild to moderate and include headache, scalp discomfort, and muscle twitching. These side effects usually go away on their own and do not require medical treatment.
There is a small risk of seizures associated with TMS, but this risk is very low, estimated to be about 1 in 30,000 treatments. Patients who have a history of seizures or who are at higher risk for seizures may not be eligible for TMS treatment.
Question 5: What should patients expect during TMS treatment?
During TMS treatment, patients sit in a comfortable chair and a small, handheld device is placed on their scalp. The device delivers magnetic pulses to the brain to stimulate nerve cells that are involved in regulating mood. The treatment session typically lasts about 30 minutes and is administered daily for several weeks.
Patient should not experience any pain during the treatment, but may feel a tapping or clicking sensation on their scalp. Patients can return to their normal activities immediately after the treatment session, and there is no recovery time or anesthesia required.
How Much Does TMS Cost? Is TMS Covered by Insurance?
In summary, Transcranial Magnetic Stimulation (TMS) is a promising treatment option for individuals struggling with depression, anxiety, and other mental health disorders. While it can be costly, many patients wonder if Medicare will cover the expense. Unfortunately, the answer is not straightforward, as Medicare’s coverage of TMS varies depending on the type of plan and the specific circumstances of the patient.
Despite the uncertainty, it is important for individuals to explore all options for receiving TMS treatment. This may include reaching out to Medicare directly to discuss coverage options, researching alternative payment plans, or considering other forms of treatment entirely. As a professional writer, I encourage patients and healthcare providers to continue advocating for accessible mental health care options and to stay informed about the latest developments in TMS research and coverage policies.
Meet Rakibul Hasan, the visionary leader and founder of Freeinsurancetips. With over a decade of experience in the insurance sector, Rakibul is dedicated to empowering individuals to make well-informed decisions. Guided by his passion, he has assembled a team of seasoned insurance professionals committed to simplifying the intricate world of insurance for you.
- Latest Posts by Rakibul Hasan
-
Can I Keep Medicaid If My Job Offers Insurance?
- -
Does Smile Direct Club Take Medicaid Insurance?
- -
Does Life Insurance Payout Affect Medicaid?
- All Posts
